This presentation provided insight on a condition caused by chronic and long term use of marijuana.
A presentation at the Center for Toxicology Pharmacology Education & Research annual conference on the Scientific Aspects of Medical Marijuana in April 2015 discussed Cannabinoid Hyperemesis Syndrome (CHS). This presentation provided insight on a condition of a cyclical vomiting illness caused by chronic and long term use of marijuana. There are many theories as to why marijuana has this effect on certain users and not others. Many of the theories suggest that various cannabinoid receptors may have slight variations from person to person with differing reactions to cannabis toxicity. CHS was first described in 2004 through the evaluation of a small case series in Australia and later in 2012 with a larger cohort in the United States.
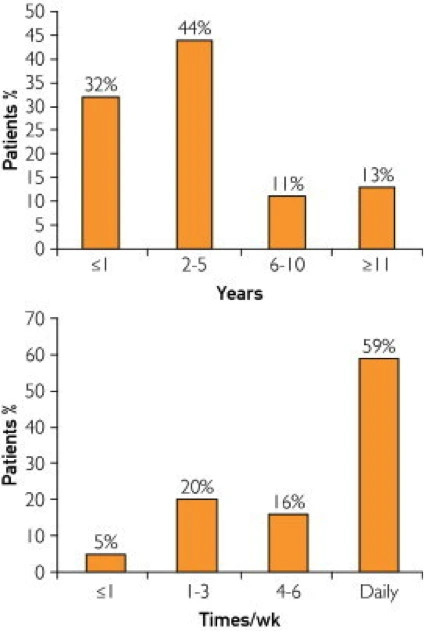
The larger U.S. study provided significant reasoning to the promotion of wider recognition and understanding of CHS as a potential danger to the use of marijuana. The graphs below show the duration (top) and frequency per week (bottom) of cannabis use prior to symptom onset. This indicates significant correlation with heavy marijuana use and CHS symptoms and diagnoses considering other potential diagnoses have been out ruled. Research also discusses CHS diagnosis among pregnant women and children noting that cessation or extreme reduction in cannabis use relieves symptoms.
Development of CHS tends to occur in stages: prodromal phase, hyperemetic phase, and recovery phase. The prodromal phase can last for months or years and consists of the development of early morning nausea, a fear of vomiting, and abdominal discomfort. Increased marijuana use during this phase is common as it is commonly believed that use will relieve nausea. Eating patterns remain normal. The hyperemetic phase presents with intensely persistent nausea, vomiting, and retching, which are often described as overwhelming and incapacitating. Eating patterns change and food aversion may develop in fear of triggering symptoms. Patients may experience abdominal pain, weight loss, and dehydration. Frequent or long hot showers are reported in an attempt to relieve symptoms. Patients present to doctor or emergency departments during this phase undergoing extensive diagnostic work-up with no avail to potential causes of symptoms. The recovery phase begins with cessation of cannabis use at which point symptoms are alleviated. Normal eating habits return, lost weight is regained, and bathing frequency returns to normal. This phase can last days, weeks, or months depending on the length of time the patient avoids cannabis use.
Official diagnosis for CHS has not yet been established, however, general guidelines have developed as the condition is identified more regularly in clinical studies and settings. General criteria for CHS diagnosis includes long term cannabis use, severe cyclic nausea and vomiting, abdominal pain and generally occurs in those under the age of 50. Symptoms are predominantly more common in the morning and generally do not affect bowel habits. CHS can be considered a valid diagnosis contingent with negative laboratory, radiographic and endoscopic test results that eliminate other potential diagnoses or causes for symptoms. The case studies indicate that hot showers and baths, when symptomatic, can temporarily alleviate symptoms. This is likely due to cannabis toxicity and its ability to disrupt the thermoregulatory systems in the brain otherwise known as the body’s ability to maintain its core internal temperature. Repeated vomiting caused by CHS can lead to esophageal damage, tooth decay, dehydration and even kidney injury or damage. Cannabis abstinence permanently relieves symptoms. Symptoms can and generally do recur when restarting cannabis use.
- Allen, J. H., de Moore, G. M., Heddle, R., & Twartz, J. C. (2004). Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut, 53(11), 1566–1570. http://doi.org/10.1136/gut.2003.036350
- Simonetto, D. A., Oxentenko, A. S., Herman, M. L., & Szostek, J. H. (2012). Cannabinoid Hyperemesis: A Case Series of 98 Patients. Mayo Clinic Proceedings, 87(2), 114–119. http://doi.org/10.1016/j.mayocp.2011.10.005
- Sun, S., & Zimmermann, A. E. (2013). Cannabinoid Hyperemesis Syndrome. Hospital Pharmacy, 48(8), 650–655. http://doi.org/10.1310/hpj4808-650 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3847982/pdf/hpj4808-650.pdf